The Essential Guide to Fibromyalgia: Symptoms, Causes, Treatments, and Natural Approaches

What Are the Types of Fibromyalgia?
Fibromyalgia is generally considered a single medical condition, but with varying symptoms and coexisting conditions, it can manifest differently from one person to another.
- Primary: Primary fibromyalgia is idiopathic, meaning it is spontaneous. It is the more common form of fibromyalgia, often diagnosed when there is no associated underlying disorder that could explain the various symptoms associated with fibromyalgia.
- Secondary: Secondary fibromyalgia occurs when there is another clinically important and dominant medical disorder, such as rheumatic, ankylosing spondylitis, lupus, irritable bowel syndrome, trauma, and surgery.
Although there are no standardized classifications, doctors may also consider variations and subgroups when diagnosing and managing fibromyalgia, often based on specific symptoms and characteristics. These subtypes are not officially recognized in clinical practice but are studied to better understand the condition.
What Are the Symptoms and Early Signs of Fibromyalgia?
Symptoms of fibromyalgia can differ vastly among individuals. Fortunately, these symptoms don’t harm organs and are not life-threatening. However, if not properly managed, they can significantly lower the person’s quality of life. Some of the primary symptoms include:
- Widespread pain: This is the most common symptom. Chronic pain and sometimes stiffness can be felt throughout the body or at multiple sites. It typically affects muscles, ligaments, and tendons and can originate from one area but may be felt in any part of the body, varying in intensity and sensation from mild to severe, including burning, soreness, stiffness, aching, or gnawing discomfort. Others may endure persistent pain throughout the day. The pain might intensify during physical activity, exposure to cold weather, or periods of high stress.
- Stiffness and achiness: Individuals with fibromyalgia often experience body stiffness and achiness in the morning. Sometimes, symptoms of stiffness, aches, and pain improve throughout the day but worsen at night.
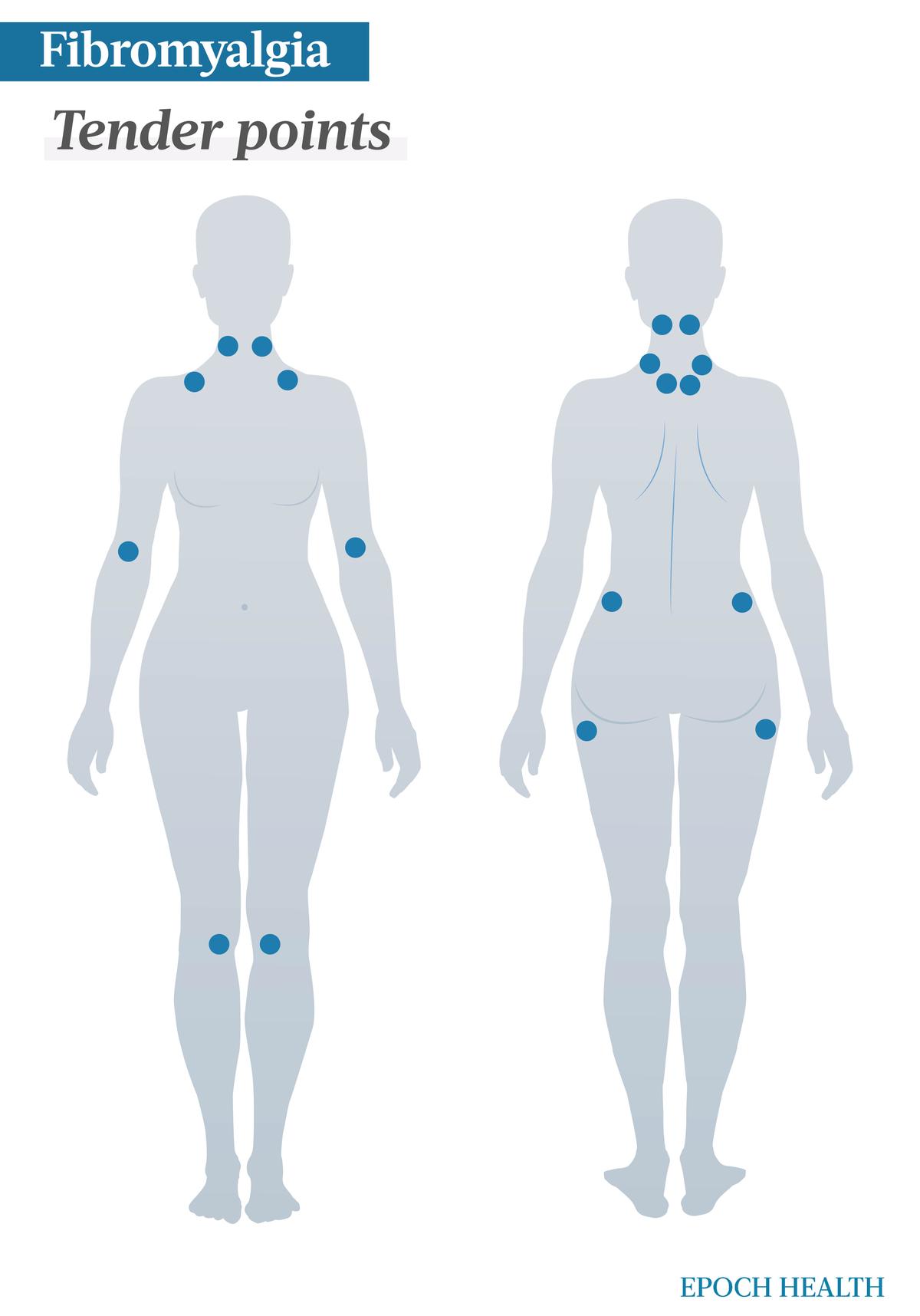
- Tender points: Tender points (also known as trigger points) are specific body sites that, when pressed, elicit pain. The pressure can be as gentle as a friendly hug. In addition, pressing a tender point can also trigger pain in a broader area, such as down the leg, arm, or back. These points come in nine pairs, with one on each side of the body, totaling 18 tender points.
- Increased pain sensitivity: This is due to a lowered pain threshold.
- Increased responsiveness to sensory stimuli: Such stimuli include temperature, light, and odors.
- “Fibromyalgia fog”: Also known as “fibro fog” or “brain fog,” this is a term used to describe a range of cognitive difficulties and mental challenges that can include memory problems, concentration issues, mental confusion, slower processing, and problem-solving speed, as well as mixing up words and details.
- Sleep disorders: Fibromyalgia patients have a high prevalence of sleep problems, which have a significant impact on lowering the pain threshold and worsening the illness’ symptoms. These sleep disorders include obstructive sleep apnea syndrome (OSAS), chronic insomnia, and restless legs syndrome (RLS), resulting in non-restorative sleep.
- Extreme fatigue: Some individuals with fibromyalgia experience chronic fatigue with constant tiredness. This fatigue can be more challenging to manage than the pain itself. It may be the result of sleep disorders associated with fibromyalgia. Even after getting eight to 10 hours of sleep, some people still wake up feeling tired and not refreshed.
- Headaches: Headaches, including migraines and tension-type headaches, are experienced by over half of patients.
- Tingling, numbness, or a burning or prickling sensation in arms and feet.
- Painful menstrual periods: However, this may actually be caused by endometriosis, a condition in which tissue resembling the uterine lining grows outside the uterus, leading to significant pelvic pain and potential fertility problems. People with fibromyalgia are more prone to developing endometriosis.
- Digestive issues, including irritable bowel syndrome (IBS), constipation, and diarrhea.
- Anxiety or depression.
- Overactive bladder.
- Temporomandibular joint syndrome (TMJ): People with TMJ may experience some symptoms due to issues with the joint and surrounding muscles, including facial, jaw, or neck pain, jaw muscle stiffness, restricted jaw movement or jaw locking, painful clicking or popping in the jaw, as well as misalignment of upper and lower teeth.
- Decreased exercise endurance.
- Dry eyes.
- Shortness of breath.
- Difficulty swallowing.
- Palpitations.
Individuals with fibromyalgia frequently experience fluctuating symptoms. These can include “flares,” during which symptoms intensify, particularly in times of stress, such as when:
- Dealing with illness.
- Traveling.
- Encountering changes in weather.
- Experiencing fluctuations in hormone levels or medication.
- Encountering stressful situations.
Is Fibromyalgia Real?
Fibromyalgia is viewed by some, including medical professionals, as an imaginary condition or a “wastebasket” diagnosis, a catch-all label to describe a certain condition for nonmedical reasons.
- Fibromyalgia doesn’t have clear biomarkers.
- Its symptoms tend to be subjective, and the primary diagnostic criteria for fibromyalgia are based on the patient’s self-reported symptoms.
- Fibromyalgia has a wide range of symptoms, which vary from patient to patient and can change over time. This lack of consistency has made some people skeptical of the condition.
- There is a lack of clear understanding of the underlying causes and, therefore, no specific targeted treatments.
- The fibromyalgia diagnosis process is complicated and challenging, as it often involves ruling out other potential conditions that share similar symptoms. Therefore, some may see that a fibromyalgia diagnosis is reached only by exclusion.
- No specific lab or imaging tests can diagnose fibromyalgia.
Some health care providers are concerned that as fibromyalgia may be imagined, its diagnosis could mask the true underlying medical conditions from which the patient suffers. Such conditions include rheumatoid arthritis, certain autoimmune disorders, lupus, depression, and viral or bacterial infections. For this reason, some medical practitioners actually consider fibromyalgia diagnosis dangerous.
What Causes Fibromyalgia?
The cause of fibromyalgia depends on its type.
Primary
Fibromyalgia often emerges slowly and gradually, with no identifiable cause. In contrast, for some, fibromyalgia may arise following an illness, a traumatic incident, or a highly stressful or emotional event. Although the precise reason certain individuals develop fibromyalgia remains unknown, it’s probable that multiple factors are at play.
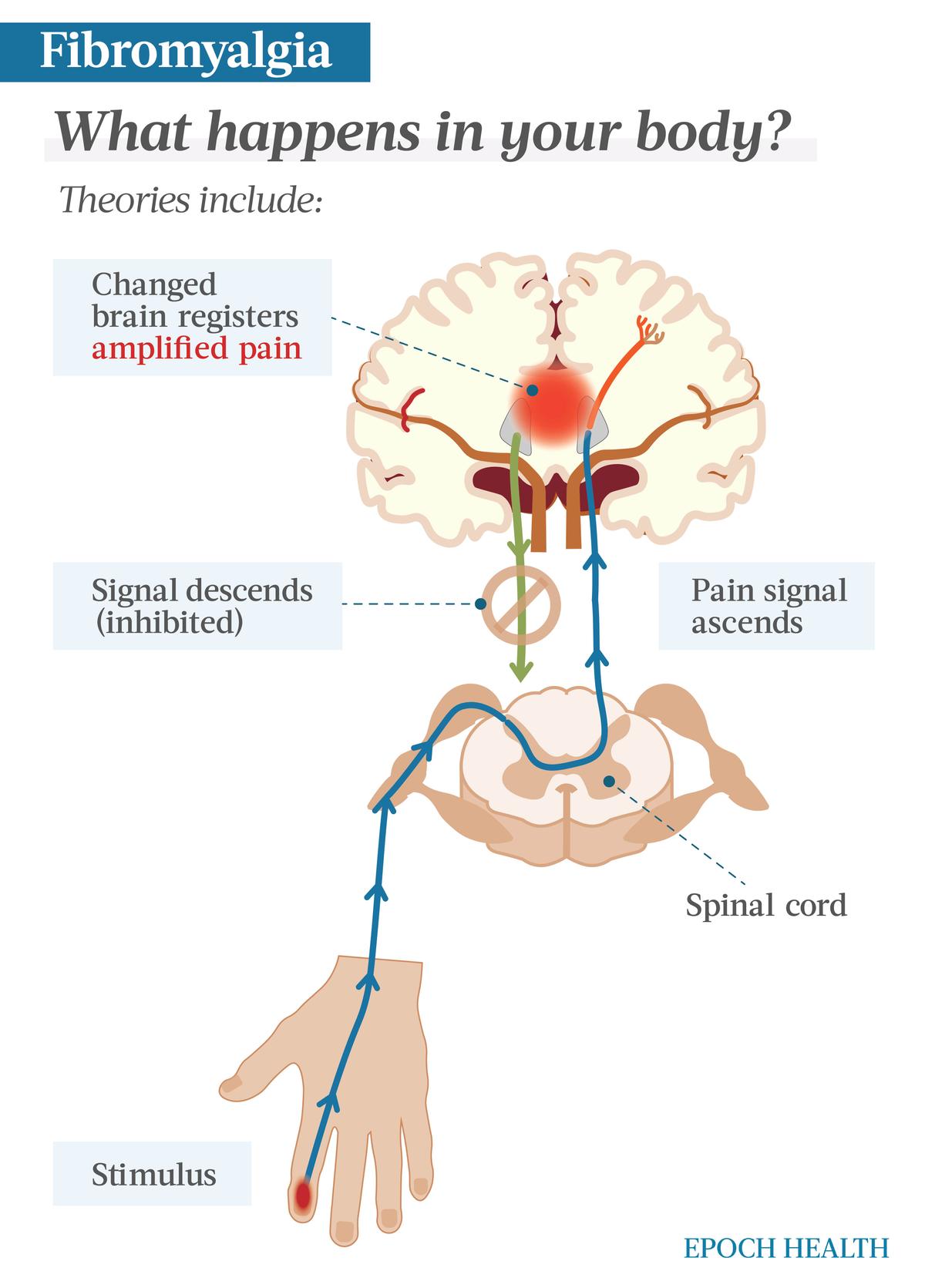
These neural pathway changes may be what plays a role in the fatigue, sleep disruptions, and cognitive difficulties frequently encountered by those with the condition.
- Genetics and family history: Genetics may play a role in fibromyalgia, but conclusive evidence is lacking. For the most part, specific genes remain unclear, but some experts believe there is a hereditary component. Individuals with a family history of fibromyalgia appear to face an increased likelihood of developing the condition themselves. According to a paper in Endotext, an online resource on endocrine disease, a person is 8.5 times more likely to develop fibromyalgia if he or she has a close relative with the condition than if he or she has a relative with rheumatoid arthritis.
- Immunity and inflammation: Growing evidence suggests that neurogenic-derived inflammatory processes in peripheral tissues, the spinal cord, and the brain contribute to the pathophysiology of fibromyalgia. This involves the release of biologically active agents like chemokines and cytokines, which activate the immune system. These processes underlie several clinical symptoms in fibromyalgia, including swelling, cognitive changes, and fatigue. Studies on patients have also confirmed the involvement of inflammation in fibromyalgia. People with this condition exhibit elevated levels of inflammatory cytokines in their circulation, including those released by immune cells. Stress and emotions are believed to be key triggers of neurogenic inflammation in fibromyalgia.
- Environmental factors: Environmental factors are believed to influence a person’s risk. These triggers may include painful conditions like acute illness, surgeries, motor vehicle accidents, or abuse that is physical or emotional.
Secondary
Secondary fibromyalgia shares similar symptoms with primary, but it is associated with an underlying chronic health condition. For instance, the following diseases can all potentially cause secondary fibromyalgia:
- Rheumatoid arthritis.
- Systemic lupus erythematosus.
- Ankylosing spondylitis.
- Osteoarthritis.
- Depression/anxiety.
- Chronic back pain.
- Irritable bowel syndrome.
Who Is More Likely to Develop Fibromyalgia?
Anyone can get fibromyalgia, but certain groups are more prone to developing it than the general population. The following are risk factors for fibromyalgia:
- Being female: In women between the ages of 20 and 55, fibromyalgia is the primary cause of generalized musculoskeletal pain, with the prevalence of fibromyalgia in women being double that in men. Studies have also shown that the prevalence of fibromyalgia in adolescents is similar to that in adults. Fibromyalgia is most common in middle-aged women due to a higher prevalence of anxiety among females, the use of ineffective coping strategies by some, changed responses to pain, increased depression levels, and hormonal fluctuations during their menstrual cycles.
- Middle- to older age: Typically, fibromyalgia initiates in midlife, and the likelihood of developing it rises with age, with it typically being diagnosed in individuals between the ages of 35 and 45.
- Depression or anxiety: Up to 50 percent of people diagnosed with fibromyalgia also have depression and/or anxiety when diagnosed, which does not mean one causes the other, but it does indicate an association.
- Family history: Since fibromyalgia tends to run in families, scientists believe that certain genes can cause fibromyalgia to develop. However, these genes remain unknown. In addition, people without a family history of fibromyalgia can also develop it.
- Underlying conditions: Secondary fibromyalgia can be the result of some rheumatic diseases, mood disorders, and sleep problems.
- Obesity.
- Repetitive injury.
- Smoking.
- Brain or spinal cord trauma: The trauma can be from physical injuries such as accidents or illnesses or emotional stress such as post-traumatic stress disorder (PTSD).
- Recent illness or infection.
- Substance abuse.
How Is Fibromyalgia Diagnosed?
There are presently no specific laboratory tests or imaging scans available for confirming fibromyalgia. The diagnosis of fibromyalgia relies mainly on the subjective perception of widespread pain throughout the body in addition to other accompanying symptoms. Given that the primary symptoms—pain and fatigue—overlap with various other medical conditions, physicians usually work to eliminate other potential causes for the symptoms.
- A widespread pain index (WPI) of 7 and a symptom severity (SS) scale score of 5, or a WPI of 3 to 6 and an SS scale score of 9.
- The symptoms have been consistently present at a similar level for a minimum of three months.
- No other underlying disorder can account for the pain.
Specifically, WPI counts the number of areas where the patient experienced pain in the past week. The score will range from 0 to 19. SS scale score assesses fatigue, morning refreshment upon waking, and cognitive symptoms over the past week using this scale: 0 = no issue, 1 = mild issues, 2 = moderate problems, and 3 = severe problems.
If you suspect you may have fibromyalgia or notice any early signs, you should consult a health care professional experienced with fibromyalgia.
- Learn about your medical history: Your doctor will discuss your medical history and symptoms, including details about pain (location, severity, duration), fatigue, and cognitive issues such as memory problems, as well as your family history of fibromyalgia (if applicable). Your concurrent medical conditions will be important in determining any other source of your pain.
- Perform a checkup: Your doctor will perform a physical exam to check if you have any signs suggesting other medical conditions, such as chronic fatigue syndrome, myofascial pain syndrome, polymyalgia rheumatica, or multiple sclerosis. This is because some of these conditions have the same/similar symptoms as fibromyalgia.
- Order certain tests for diagnosis: These tests are taken to rule out other conditions that may cause pain. X-rays and other imaging tests may also be ordered in addition to those listed below.
Diagnostic Tests
Tests, such as the following, are taken to check hormone levels and inflammation signs, providing valuable information to your doctor in making an accurate diagnosis:
- Complete blood count (CBC): This blood test measures the levels of white blood cells, red blood cells, and platelets in the blood and evaluates the patient’s oxygen-carrying capacity.
- C-reactive protein (CRP) test: A c-reactive protein test measures the CRP level in your blood, which is a protein produced by your liver. Normally, CRP levels are low, but they rise when there is inflammation in your body. Elevated CRP levels can indicate a significant health condition associated with inflammation.
- Comprehensive metabolic panel (CMP): A comprehensive metabolic panel measures 14 blood substances, including glucose, calcium, sodium, potassium, carbon dioxide, chloride, and total protein. It also measures kidney function. CMP offers insights into the body’s chemical balance and metabolism. Abnormal levels of these substances may signal a significant health issue.
- Erythrocyte sedimentation rate (ESR or sed rate): This test measures the rate at which red blood cells settle at the bottom of a test tube. In the presence of swelling and inflammation, blood proteins aggregate and become denser than usual, causing them to settle more rapidly. Typically, the faster the descent of blood cells, the more pronounced the inflammation.
- Thyroid function test (TFT): A thyroid function test typically involves measuring thyroid stimulating hormone (TSH) and thyroid hormones in the blood to assess the thyroid gland’s function and its ability to regulate hormone production.
What Are the Complications of Fibromyalgia?
According to the U.S. Centers for Disease Control and Prevention (CDC), complications of fibromyalgia may include:
- Increased hospitalization rates: Individuals with fibromyalgia are twice as likely to require hospitalization compared to those without the condition.
- Reduced quality of life
- Elevated incidence of major depression: Adults with fibromyalgia are over three times more likely to have major depression than those without the condition.
- Higher risk of suicide and injury-related deaths: Fibromyalgia patients have higher rates of suicide and injury-related deaths, but the overall mortality among adults with fibromyalgia is similar to that of the general population.
- Increased prevalence of other rheumatic conditions: Fibromyalgia frequently co-occurs with lupus and types of arthritis, such as osteoarthritis and rheumatoid arthritis.
What Are the Treatments for Fibromyalgia?
Fibromyalgia typically persists throughout a person’s life. Importantly, it is not a progressive disease, meaning it does not aggravate over time, and it does not lead to damage in the joints, muscles, or organs, either.
While there is no known cure for fibromyalgia, its symptoms can be managed and treated with medication and self-management strategies.
The health care professionals specializing in the treatment of fibromyalgia and types of inflammatory conditions, such as arthritis, are called rheumatologists. Other health care professionals who may be involved include exercise physiologists, mental health professionals, a counselor trained in talking therapies, pain management specialists, physical therapists, and sleep specialists.
While less severe cases may improve with stress reduction or lifestyle adjustments, more severe cases may necessitate a comprehensive team-based approach to treatment. Additionally, despite initial nonpharmacologic and single pharmacologic treatment at maximum tolerated doses, many patients remain symptomatic. In such cases, combination drug therapy, cognitive behavioral therapy (CBT), or other adjunct therapies may be advised.
1. Exercise and Fitness (Physiotherapy)
Physiotherapy is a science-driven approach focused on improving or reinstating the functioning of various body systems with physical remedies.
Regular exercise, particularly cardiovascular activities, is one of the most effective approaches for fibromyalgia management, as it helps with pain and improves sleep quality. The recommended cardiovascular fitness training involves at least 30 minutes of aerobic exercise three times every week.
In addition, hydrotherapy, such as water aerobics or swimming, can be used, as the water’s warm temperature and pressure can provide relief from pain, reduce inflammation, and improve physical function.
Your rheumatologist might also suggest additional gentle exercises, including yoga or light walking, to enhance muscle strength, flexibility, and endurance.
Individuals with fibromyalgia are typically advised to steer clear of activities that entail rapid, abrupt motions and high-impact exercises, such as running and jumping, although some individuals may gradually work their way up to these levels of activity.
2. Lifestyle Changes
Self-care is also an important part of fibromyalgia management. The following lifestyle changes are recommended:
- Getting sufficient sleep: Most adults should get seven to eight hours of sleep per night. Since fibromyalgia can disrupt sleep patterns, you may try to increase your sleep time and quality by having a consistent bedtime and wake time, avoiding caffeine, alcohol, and spicy meals before bedtime, avoiding daytime naps, and engaging in relaxing pre-sleep activities without screens, such as listening to soothing music or taking a warm bath.
- Managing stress: Stress reduction is necessary, as stress triggers fibromyalgia symptom flare-ups. You can use relaxation techniques, formal stress reduction programs, meditation, yoga, breathing exercises, acupuncture, massage, and talk therapies.
- Identifying and avoiding triggers: You must learn to recognize and pinpoint the “triggers” that exacerbate your symptoms, which might include weather changes, specific activities, stressors, or sleep deprivation. Then, steer clear of them or develop strategies to handle them effectively.
- Relieving pain and stiffness: This can be done with pain medication, heat or cold packs, exercise, and massage.
- Monitoring your mental state: The lifetime prevalences of anxiety disorders and depression are 60 percent and 74 percent, respectively. You should consult your doctor if you experience signs of depression or anxiety.
- Eating a balanced, anti-inflammatory diet: Although there is no specific diet for fibromyalgia, having a nutritious diet and eating foods that reduce inflammation, including leafy green vegetables, dark yellow vegetables, fruits, and whole grains, can be beneficial to your fibromyalgia symptoms and overall health. Inflammatory foods may include red—but especially processed—meat, commercial baked goods, pastry made with refined flour, deep-fried foods, foods with a lot of added sugar, processed foods made with seed oil, and foods containing trans fats.
- Avoiding smoking: In fibromyalgia patients, smoking is linked to cognitive dysfunction and increased symptom severity, reduced quality of life, sleep issues, and increased anxiety when compared to nonsmokers. Therefore, avoiding smoke is important for individuals with fibromyalgia.
- Adjusting work demands: Working is beneficial to your health, but you should avoid becoming too stressed and take regular breaks during work. You can consult your doctor or an occupational therapist for help in this regard.
3. Medications
Although some patients may achieve sufficient relief through nonpharmacological methods alone, for the majority of fibromyalgia patients, combining nonpharmacological approaches with medications is advised.
Since conventional treatments like pain medication may not always provide relief for individuals with fibromyalgia, they may need to experiment with multiple medications before discovering the most effective one, and they might notice that a medication that initially alleviated their symptoms becomes less effective with time.
- Antidepressants: Antidepressants are commonly prescribed for fibromyalgia to alleviate pain and fatigue by increasing certain brain neurotransmitters, reducing sensitivity to pain. Treatment typically begins with tricyclic antidepressants. One class, known as serotonin and norepinephrine reuptake inhibitors (SNRIs), raises serotonin and norepinephrine levels. Duloxetine and milnacipran are SNRIs. In addition, tricyclic antidepressants such as cyclobenzaprine enhance neurotransmitter levels and promote sleep. In cases where patients have an inadequate response or cannot tolerate tricyclic antidepressants, SNRIs or anticonvulsants are considered as alternatives.
- Analgesics (pain-relievers): Pain medications such as acetaminophen (also known as paracetamol) and ibuprofen can provide temporary pain relief. Anti-inflammatory pain medications are often ineffective for fibromyalgia as it doesn’t typically involve tissue inflammation. However, they may provide relief for other concurrent painful conditions. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen and naproxen, can alleviate deep muscle and joint pain from fibromyalgia. NSAIDs may be more effective when used in combination with other fibromyalgia medications. Extended, high-dose NSAID usage can raise the risk of heartburn, gastrointestinal bleeding, and complications in the cardiovascular, kidney, and liver systems, as well as fluid retention.
- Anticonvulsants: Anticonvulsants such as pregabalin can alleviate fibromyalgia pain by calming overactive nerve cells that transmit pain signals and may improve sleep. Side effects may include drowsiness, dizziness, fluid retention, and weight gain. Fibromyalgia patients can also use them to alleviate pain and enhance sleep quality, as they function by disrupting the transmission of pain signals to the brain.
- Muscle relaxants: Muscle relaxants can also alleviate pain and improve sleep in individuals with fibromyalgia. Their common side effects include dizziness, drowsiness, blurred vision, difficulty urinating, constipation, and dry mouth.
4. Talk Therapy and Counseling
Psychotherapy, often referred to as talk therapy, encompasses a range of treatments designed to assist individuals in recognizing and modifying distressing emotions, thoughts, and behaviors, to manage pain, stress, and negative thoughts. A few options include:
- Cognitive behavioral therapy (CBT): CBT is a form of counseling that concentrates on modifying specific thought patterns and behaviors to manage the symptoms of a condition. There is evidence indicating that CBT can be effective in reducing pain and disability associated with fibromyalgia.
- Acceptance and commitment therapy (ACT): Acceptance and commitment therapy involves learning to embrace what you cannot control and committing to changes that enhance your life. ACT has demonstrated effectiveness in enhancing sleep quality, alleviating pain, and addressing negative thoughts and emotions.
5. Transcranial Direct Current Stimulation (tDCS)
Transcranial direct current stimulation (tDCS) is a widely used brain stimulation technique that can either enhance or inhibit various behaviors by adjusting cortical excitability. tDCS has shown promise in treating chronic pain such as that caused by fibromyalgia.
How Does Mindset Affect Fibromyalgia?
Fibromyalgia appears to have a more substantial relationship to mentality and psychological characteristics than many other physical conditions. While trauma and high stress can trigger fibromyalgia, a negative mindset, adverse mental conditions, and temperament can all affect the condition’s severity, according to a 2019 article in Psychology Research and Behavior Management. Additionally, extraversion in fibromyalgia patients is also associated with lower levels of anxiety, depression, and pain, suggesting a person’s personality and approach to his or her condition may offer protective effects.
- Stress reduction: Maintaining a positive outlook can help reduce stress, which is known to exacerbate fibromyalgia symptoms.
- Decreased pain: Psychological and emotional factors, including one’s perception of pain, may influence the experience of pain. A positive mindset can lead to positive emotions, potentially leading to pain reduction.
- Reduced depression: A positive mindset can lift the patient from depression and give him or her a sense of well-being.
- Promote treatment adherence: Patients with a positive outlook may be more motivated to adhere to their treatment plans.
What Are the Natural Approaches to Fibromyalgia?
Many of the alternative and complementary therapies recommended by medical professionals are as follows:
1. Acupuncture
Acupuncture is a traditional Chinese medical practice that involves the insertion of thin needles into specific points on the body. According to a meta-analysis, acupuncture therapy appeared to be a safe and effective approach for fibromyalgia patients. In another meta-analysis, low-to-moderate evidence was found that acupuncture might bring certain health benefits to individuals with the condition.
2. Supplements
Many supplements have demonstrated efficacy in relieving fibromyalgia symptoms. However, they may not be suitable for all patients, as they may have side effects and interactions with other medications that you’re taking. In addition, unlike drugs, they don’t require FDA approval before being sold. Consult your doctor before trying any supplements.
- Omega-3 fatty acids (fish oil): Renowned for its anti-inflammatory attributes, incorporating a high-quality fish oil supplement can potentially reduce inflammation and pain while enhancing immune system function.
- Vitamin D: Some studies found that taking vitamin D supplements by fibromyalgia patients could result in pain reduction.
- Acetyl L-carnitine: Also known as ALCAR, acetyl L-carnitine is a modified form of the amino acid carnitine. It plays a role in energy production in the body. Initial findings of a study indicated that ALCAR may also be effective in reducing depressive symptoms and pain and enhancing the quality of life for individuals with fibromyalgia.
- Magnesium citrate: Some studies suggest that magnesium deficiency, which affects muscle energy levels, might be connected to fibromyalgia development. In one study, women who received 300 milligrams of magnesium citrate daily for eight weeks saw improvements in their tender points, depression, and anxiety.
- S-adenosylmethionine (SAMe): S-adenosylmethionine is naturally synthesized in the body from methionine, an amino acid present in foods, and it has been discovered to regulate essential functions in living cells. One study indicated that SAM-e might offer benefits for individuals with fibromyalgia, with the suggested dosage being 800 milligrams per day.
- Coenzyme Q10 (CoQ10): Coenzyme Q10 is an energy-converting compound and a potent antioxidant present in nearly all cells in the body. In a randomized trial, 20 fibromyalgia patients took 300 milligrams of CoQ10 daily for 40 days, resulting in a notable reduction in pain, tender points, fatigue, and morning tiredness, as well as enhancements in antioxidant enzyme activity and mitochondrial function.
- Melatonin: Melatonin, the sleep hormone produced by the pineal gland each night, not only promotes restful sleep but also offers antioxidant benefits. One study found that melatonin may help improve fibromyalgia-related pain, pain threshold, and sleep quality.
3. Herbs
Certain herbal therapies may also alleviate the symptoms of fibromyalgia, including the following:
- Ginger (Zingiber officinale) root: Ginger root contains active compounds known as gingerols and shogaols, which have pain-relieving and anti-inflammatory properties. The results of one animal study suggested that when mice with fibromyalgia-like muscle pain consumed ginger roots daily, the pain relief medication worked better, and their inflammation and memory issues linked to chronic pain improved.
- Ginseng (Panax ginseng): Ginseng contains special compounds called ginsenosides that can relieve pain. In one study, ginseng extract appeared to help reduce the number of tender points and improve quality of life in fibromyalgia patients compared to baseline values, but researchers couldn’t definitively conclude that the treatment was more effective than placebo.
- Turmeric (Curcuma longa): Turmeric contains curcumin, a polyphenol with antioxidant, anti-cancer, and anti-inflammatory properties. A study involving the use of the curcumin medication known as Flexofytol was conducted on patients with fibromyalgia. The results showed that 41 out of 62 patients had experienced health benefits from this medication.
- Capsicum or capsaicin (Zostrix): Capsaicin is one of the chemical compounds found in chili peppers responsible for the spicy or hot sensation when consumed or applied to the skin. It is commonly used as a pain relief treatment in various forms, such as creams, liquids, patches, and even some dietary supplements. As per one study, severely affected fibromyalgia patients experienced short-term relief by applying a 0.075 percent capsaicin cream three times a day for six weeks.
4. Chiropractic Therapy
Chiropractic therapy focuses on diagnosing and treating mechanical disorders of the musculoskeletal system. Chiropractors use manual manipulation and adjustments of the spine and other parts of the body to alleviate pain and improve function.
5. Massage
Massage therapy involves hands-on manipulation of the body’s soft tissues to promote relaxation and alleviate pain. It typically includes techniques such as kneading, rubbing, and applying pressure to muscles and connective tissues.
6. Mind-Body Practices
- Mindfulness practice: In one study, after participating in one Mindfulness-Based Stress Reduction (MBSR) program, a group of fibromyalgia patients experienced significantly decreased perceived stress, sleep disturbance, and symptom severity.
- Tai chi and qigong: Tai chi, derived from ancient Chinese martial arts practices, involves slow, gentle movements, meditation, and controlled breathing. Qigong is a centuries-old Chinese practice that aims to optimize energy in the body, mind, and spirit to improve overall health and well-being. Both practices can reduce stress and help fibromyalgia patients relax. Specifically, in one study, tai chi showed similar or better improvement in fibromyalgia symptoms compared to aerobic exercise, which is a very common existing treatment. In addition, longer tai chi sessions led to greater improvements. Also, as per one review, in four studies comprising 201 participants who consistently practiced for 30 to 45 minutes of qigong daily over six to eight weeks, noticeable improvements in pain, sleep, daily life impact, and both physical and mental function were observed. These benefits were sustained for four to six more months.
- Yoga: Yoga is also superb in reducing stress and promoting overall well-being. In one case study, the participant practiced special yoga postures for one hour daily, six days a week, for nine months. She experienced reduced muscle fatigue and improved quality of life and sleep as a result.
How Can I Prevent Fibromyalgia?
Unfortunately, fibromyalgia cannot be definitively prevented, as its exact cause is not fully understood, and it may have a genetic component. However, the self-care strategies used to treat the condition can help reduce the risk of developing fibromyalgia, including:
- Regular exercise.
- Stress management.
- Balanced and nutritious diet.
- Adequate sleep.
- Avoidance of overexertion.
- Maintenance of emotional well-being.
If you are at risk due to family history or other factors, consider discussing preventive measures with a health care professional.
Source: Epoch Times
Please Donate Below To Support Our Ongoing Work To Expose The Lies About Covid 19
PRINCIPIA SCIENTIFIC INTERNATIONAL, legally registered in the UK as a company  incorporated for charitable purposes. Head Office: 27 Old Gloucester Street, London WC1N 3AX.
incorporated for charitable purposes. Head Office: 27 Old Gloucester Street, London WC1N 3AX.
Trackback from your site.
